Introduction:
Thrombocytopenia and autoimmune hemolytic anemia (AIHA) are extra-criteria manifestations of antiphospholipid syndrome (APS). They have a higher incidence in secondary cases, and there is little information on primary antiphospholipid syndrome (pAPS).
Aim:
To evaluate the clinical characteristics and profile of antibodies in pAPS with hematological activity.
Material and methods:
A retrospective study included patients with pAPS, diagnosed according to the Sapporo criteria with follow-up at third level of care in Mexico City from 1990 to 2021. Descriptive statistics were used, and chi-squared test, Mann-Whitney U test, and logistic regression were performed.
Results:
A total of 97 patients with pAPS were included; 73.2% (71) were women with a mean age of 33.9 + 11.5 years and a mean follow-up of 132 months (24-360).
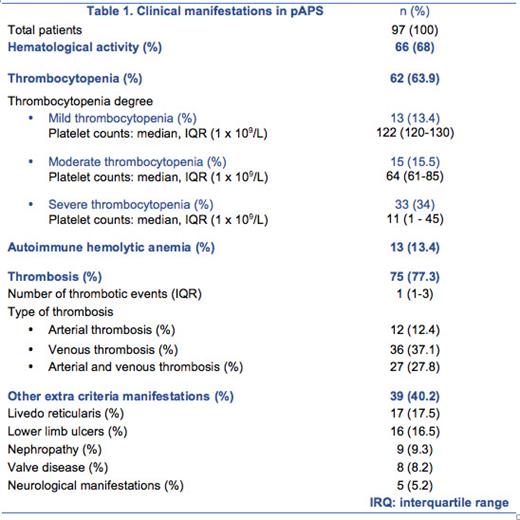
We found that 77% (75) presented thrombotic and 37% (36) obstetric manifestations. In 68% (66) of patients, hematological manifestations (non-exclusive groups) were found. Further, 63.9% had thrombocytopenia, the most common kind being severe, and a minority had AIHA in 13.4%. Table 1 describes the clinical manifestations.
Patients with thrombocytopenia were younger, with 32 + 10.3 years vs 37 + 13 years ( p = 0.046). A total of 59.7% (37) had a triple marker. In comparison with patients without thrombocytopenia, 69.4% (43) presented positive lupus anticoagulant vs 48.6% ( p = 0.043) and OR 2.5 (CI 95% 1.06-6.1). An 83.9% (52) had positive IgG anticardiolipin vs 62.9% ( p = 0.019), OR 3.21 (CI 95% 1.19-8.63) with a higher titer of 19.4 vs 6.1 ( p = 0.017) and OR 1.01 (CI 95% 0.99-1.04). They had higher titers of antiβ2 glycoprotein-I IgM of 6.8 vs 5.2 ( p = 0.019) with OR 1.03 (CI 95% 0.99-1.06) and of antiphosphatidyl serine/prothrombin IgM of 52.8 vs 16.8 ( p = 0.004), OR 1.01 (CI 95% 1- 1.02).
In patients with AHAI, anti-β2 glycoprotein-I IgM antibody titers of 7.1 vs 5.9 were identified, which were higher compared with those who did not present it ( p = 0.026).
Those without hematological activity had more thrombosis ( p < 0.001). When comparing the groups with and without thrombosis, we observed that those with thrombosis had lower titers of antiβ2 glycoprotein-I IgM in 5.8 vs. 7.4, p = 0.036, OR 0.97 (CI 95% 0.94-1) and higher anti-phosphatidyl serine/prothrombin titers in 61.2 vs 12.1, p = 0.021 with OR 1.02 (CI 95% 1-1.04).
A total of 76.3% (74) received anticoagulant and 24.7% (24) received antiplatelet. Immunosuppression was prescribed in 38.1% (37). Those with severe thrombocytopenia received: prednisone in 54.5% (18) of cases, methylprednisolone in 36.4% (12), rituximab in 3% (1), and splenectomy in 36.4% (12). In patients with AHAI, 84.6% (11) received immunosuppressants and 46.2% (6) underwent splenectomy.
Conclusion:
A higher incidence of hematological activity was identified in pAPS, mostly in young women. The most common kind was severe thrombocytopenia, as opposed to what was described in literature as mild to moderate.
Differences were found regarding the titer and positivity of antibodies. With thrombocytopenia, there was a higher frequency of positive lupus anticoagulant, anticardiolipin IgG and antiβ2 glycoprotein-I IgM with higher titers. Patients had anti-phosphatidyl serine/prothrombin antibodies as an extended panel and a correlation with hematological activity was identified.
Knowing the serology of pAPS is useful to identify in good time patients who may present severe hematological manifestations. No patient died of a hematologic complication; however splenectomy was required in some cases. To our knowledge this is one of the few studies that evaluate hematological manifestations in pAPS.
Disclosures
Orozco Collazo:Janssen: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal